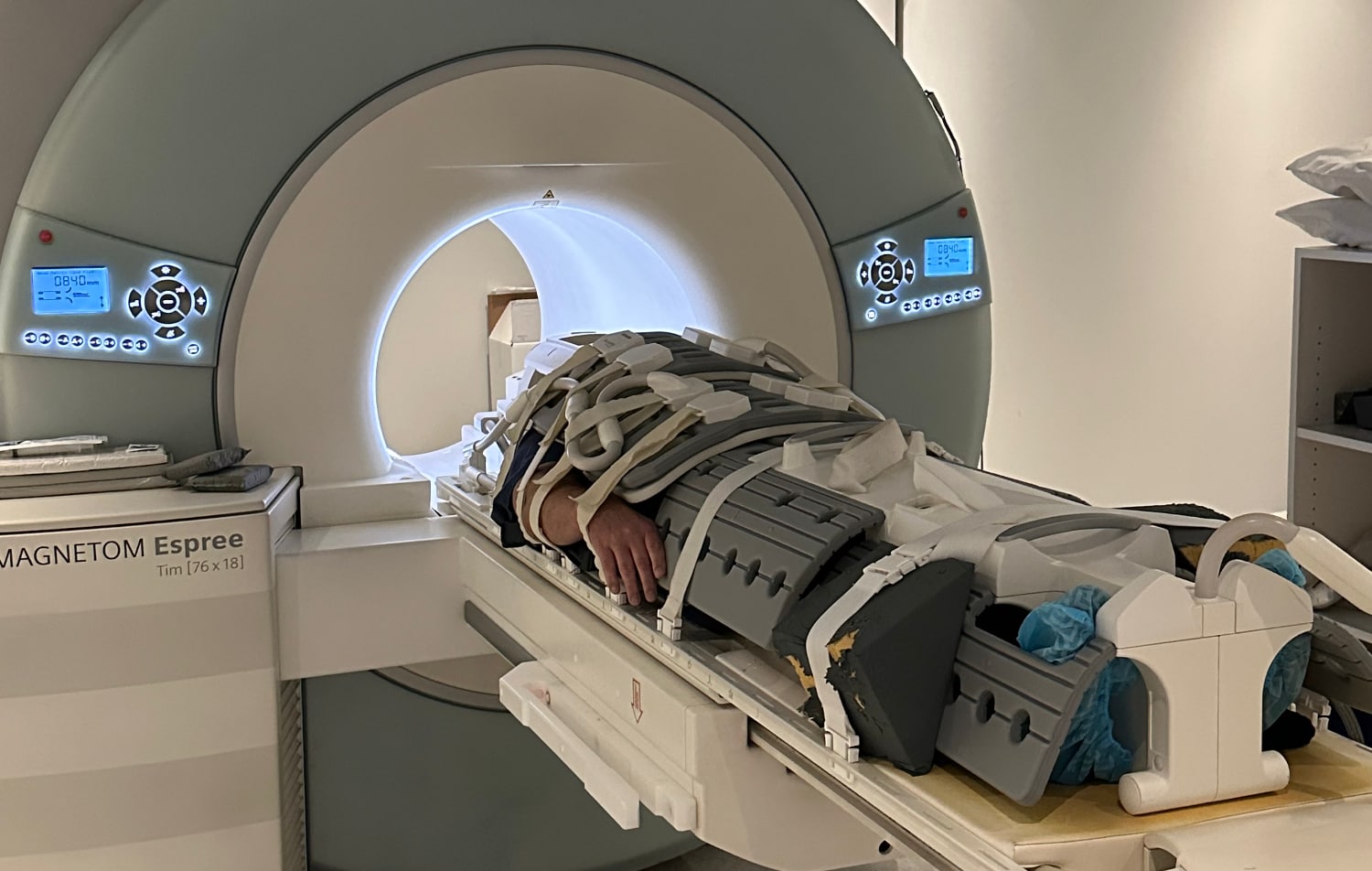
Structural or functional MRI imaging has been investigated for its potential to improve outcomes for patients receiving rTMS treatment. Our research team has led much of this research, commencing with a pivotal trial back in 2009 that showed that we could use structural MRI scans - those that take a picture of the structure of the brain, rather than its function - as part of the setup for rTMS treatment.
We found that using MRI scans would produce better clinical outcomes than localising treatment with the way that was being used at that time. It is important to note, however, that the standard approach at that time localised TMS treatment without taking differences in head size between individuals into account.
We now use more sophisticated methods that take head size into account and which have consistently been shown to produce more reliable localisation of the TMS coil. These new methods also result in the coil being placed somewhat further forward, to a more effective treatment site, than our old methods.
In recent years there has been considerable excitement about, and research into, methods for using functional MRI scans to localise TMS treatment. These are scans that analyse patterns of brain activity, rather than just brain structure. However, these studies tend to indicate that treatment should be localised at about the same area of the brain that we are already providing treatment to now, one that is further forward than the one that was used previously. In other words, this sort of imaging would improve how we were treating patients back in the early 2000s, but we have already adjusted our targeting in a way that achieves the same effect. No studies have shown the benefits of MRI-based targeting over these new methods that we now use.
Therefore, there is absolutely no evidence that using MRI targeting produces better clinical outcomes than those being achieved with current treatment approaches. We do not use these as they are costly, add to the complexity of treatment and provide an additional source of error that could result in actually less reliable treatment if used widely in clinical practice.
What about the use of EEG?
This is an approach that measures electrical brain activity, which is related to the way the brain functions and processes information. We have been heavily involved in research exploring whether we can use EEG methods to predict which patients will respond to TMS and to help determine the frequency of stimulation being used. However, despite the promise of this area, it is clearly too early to promote EEG-based TMS as being any better than what we currently do or even being equivalent. There are no substantive clinical trials demonstrating that EEG-based TMS is more effective, or even equivalent to, standard treatment approaches.
Unfortunately, both of these areas are ones where it is possible to make extravagant and exciting claims about improved treatment methods that are impossible for patients to know and are based more on excitement and hype than on actual science. At this stage, these are areas of great promise but not where there is any evidence of improved outcomes.