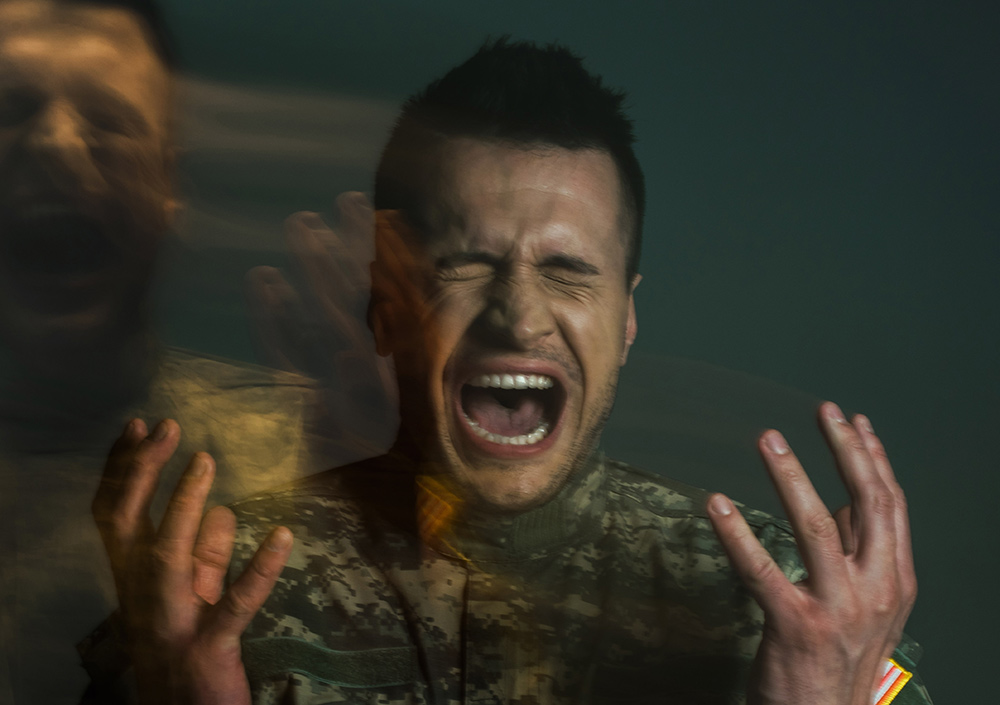
Returning to civilian life after military service brings many challenges, and for many former service members, mental health is one of the most difficult hurdles to face. Veterans and mental health are closely linked, with higher rates of post-traumatic stress disorder (PTSD), depression, and anxiety compared to the general population. While medication and therapy can help, they don’t always provide lasting relief from depression and PTSD symptoms. That’s why an increasing number of veterans are turning to Transcranial Magnetic Stimulation (TMS) therapy—an innovative, medication-free treatment offering new hope for recovery.
The Mental Health Challenges Veterans Face
Many Australian veterans experience ongoing mental health issues long after their military service ends. Research shows that PTSD affects over 17% of ex-serving ADF personnel, with many also struggling with co-occurring conditions such as depression, anxiety, and substance use. Veteran PTSD symptoms may include nightmares, flashbacks, hypervigilance, emotional detachment, and intense irritability—often disrupting work, relationships, and daily functioning.
While traditional treatment options like medication and psychological therapy are often effective, they don’t work for everyone. Some veterans find side effects intolerable, while others report little or no symptom relief even after years of therapy. For these individuals, a new approach to veteran PTSD therapy may be the breakthrough they’ve been searching for.
How TMS Therapy Can Benefit Veterans
Veterans often carry invisible wounds from their service—trauma that doesn’t respond to medication alone. TMS therapy offers a new, research-backed option for veterans with treatment-resistant PTSD and depression.
Here’s why it’s particularly effective for veteran PTSD therapy:
1. Drug-free and non-invasive
Many veterans prefer to avoid long-term medication due to side effects, health concerns, or personal beliefs. TMS provides an effective, non-pharmacological alternative.
2. Fewer side effects
Unlike antidepressants, which can cause fatigue, weight gain, or emotional blunting, TMS has minimal side effects. Most patients only report mild scalp discomfort or headaches, which typically fade after the first few sessions.
3. Proven effectiveness
Multiple studies, including a 2019 trial in The Lancet Psychiatry, show that TMS significantly reduces PTSD symptoms, especially in those who haven’t responded to other treatments.
4. Supports brain rewiring
TMS promotes neuroplasticity—the brain’s ability to form new connections. This is essential for healing from trauma and managing long-term symptoms.
5. Complements other treatments
TMS can be used alongside trauma-informed therapy and counselling, or with medication if needed. In fact, combining approaches often leads to better results, as therapy helps process memories while TMS strengthens brain function.
What to Expect During Treatment
TMS therapy for PTSD usually involves five sessions per week over a period of four to six weeks. Each session lasts between 20 and 40 minutes. During treatment, you’ll sit in a comfortable chair while a magnetic coil is placed against your scalp. The procedure is painless, though you may feel a tapping sensation.
Some people notice improvements within two to three weeks, while others see changes closer to the end of their treatment course. The effects build over time, and follow-up reviews help track your progress.
Is TMS Right for All Veterans?
While TMS is safe and effective for many, it’s not suitable for everyone. You may not be eligible if you have:
- Metal implants near the head or neck (excluding dental work)
- A history of seizures or epilepsy
- Certain neurological conditions
- Severe movement disorders or unmanaged psychosis
A comprehensive clinical assessment is essential to determine your suitability and ensure TMS can be delivered safely.
How to Help a Veteran with PTSD
Supporting someone through PTSD can be challenging, especially when symptoms are severe or persistent. If you’re wondering how to help a veteran with PTSD, start by encouraging them to seek professional care. Be patient, avoid judgement, and learn about the symptoms so you can better understand their experience.
You can also explore new treatment options together, like TMS therapy. Having someone on their side—whether it’s helping to organise appointments or simply listening—can make a real difference.

Support Through Monarch Mental Health Group
At Monarch Mental Health Group, we provide compassionate, evidence-based care for veterans and others living with PTSD and depression. Our psychiatrist-led clinics across New South Wales, Victoria, and Queensland offer advanced treatment options, including repetitive and deep TMS therapy, next step medication services, and psychological support tailored to the individual.
Our team understands the complexities of veteran PTSD symptoms and the importance of personalised care. Through research-backed approaches and a focus on real recovery, we help veterans find hope beyond medication.
If you or a loved one is seeking TMS therapy for PTSD or exploring alternatives when other treatments haven’t worked, we’re here to help. Contact Monarch Mental Health Group today to arrange an assessment. A referral from your GP or psychiatrist is required for Medicare rebates.
FAQs
What is TMS therapy and how does it help veterans?
Transcranial Magnetic Stimulation (TMS) is a non-invasive therapy that uses magnetic pulses to stimulate brain regions involved in mood and emotional regulation. For veterans experiencing PTSD or depression, TMS helps restore healthy brain activity without the need for medication. Monarch Mental Health Group offers TMS as part of a tailored treatment plan, available at our clinics across NSW, Victoria, and Queensland.
How is TMS different from medication?
Unlike medication, which affects the whole body, TMS directly stimulates specific areas of the brain. It has fewer systemic side effects and doesn’t require daily pills. For veterans with mental health conditions who don’t respond well to antidepressants, TMS treatment can be a valuable alternative. Monarch’s clinics across Australia offer this non-drug approach as part of our commitment to personalised, evidence-based care. Contact us today.
How long does TMS treatment take?
TMS therapy for PTSD or depression typically involves five sessions per week for 4–6 weeks. Each session lasts around 20–40 minutes, and no recovery time is needed. Monarch Mental Health Group offers flexible appointments across our clinics to fit treatment into your schedule. Speak to us today for more information.
Will I need to stop my current PTSD or depression treatment to start TMS?
Not necessarily. TMS treatment for PTSD can often be used alongside your current medication or therapy. At Monarch Mental Health Group, our clinical team will review your treatment plan and work with your GP or psychiatrist to coordinate care at our clinics in New South Wales, Victoria, and Queensland.
What results can veterans expect from TMS therapy for PTSD or depression?
Many veterans begin to notice improvements in mood, sleep, and emotional stability within a few weeks. Results vary, but studies show lasting benefits, especially for those with treatment-resistant symptoms. Monarch Mental Health Group tracks progress closely to adjust your treatment as needed.
.png)
About The Author
Dr Ted Cassidy
Dr. Ted Cassidy is a psychiatrist and co-founder of Monarch Mental Health Group in Australia, which provides innovative treatments for depression, PTSD, and anxiety. Monarch Mental Health is recognized as Australia's first outpatient clinic offering assisted therapy and is the largest provider of outpatient magnetic stimulation therapy.