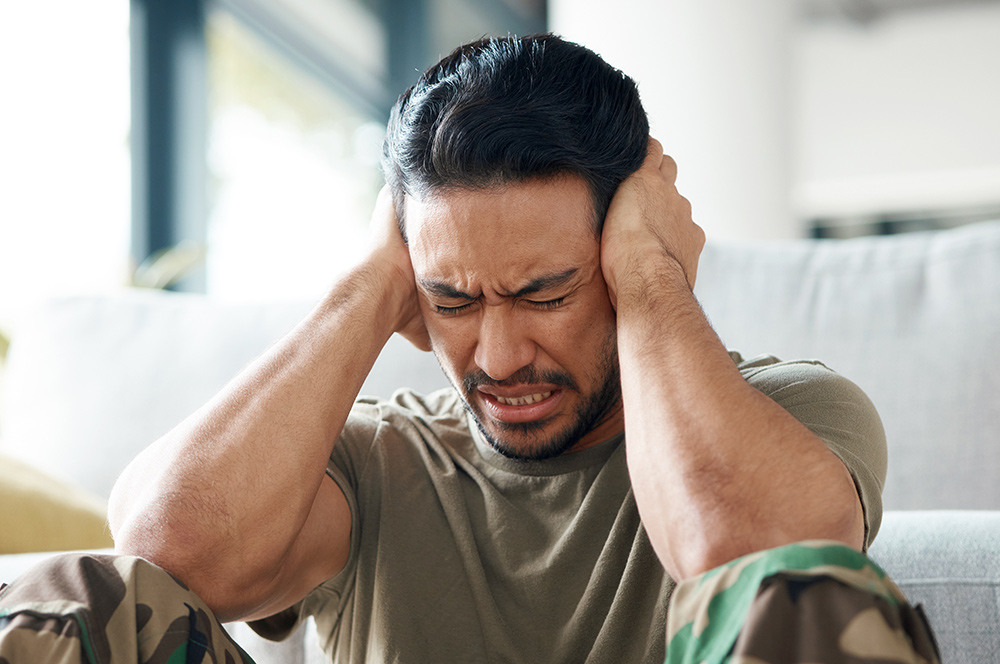
Post-Traumatic Stress Disorder (PTSD) is a serious and complex mental health condition that affects many military veterans worldwide. The intense and often life-threatening experiences encountered during active service can leave lasting psychological scars, leading to distressing symptoms such as flashbacks, nightmares, emotional numbness, and heightened anxiety. Without proper treatment, PTSD from a traumatic event can severely impact a veteran’s quality of life, relationships, and overall well-being. Thankfully, numerous evidence-based treatment options exist, offering hope and healing for those who have served.
Understanding PTSD Symptoms in Veterans
Post-Traumatic Stress Disorder develops following exposure to one or more traumatic events, such as combat, military accidents, or witnessing death. PTSD symptoms typically fall into four categories:
- Intrusive Thoughts – Unwanted distressing memories, flashbacks, and nightmares.
- Avoidance – Steering clear of places, people, or situations that trigger painful memories.
- Negative Changes in Thinking and Mood – Feelings of guilt, detachment, or loss of interest in previously enjoyed activities.
- Hyperarousal – Heightened alertness, irritability, difficulty sleeping, and exaggerated startle responses.
While PTSD symptoms can be debilitating, veterans should know that they are not alone and that help is available through various therapeutic and medical interventions for this and associated mental health conditions such as anxiety and depression.

Evidence-Based Treatments for PTSD in Veterans
There is no one-size-fits-all approach to treating PTSD, but several scientifically backed treatments have shown significant success in helping veterans who develop PTSD to regain control over their lives.
1. Cognitive Behavioural Therapy (CBT)
CBT is a widely used psychotherapy that helps individuals recognise and change harmful thought patterns that contribute to PTSD. Two specific forms of CBT are particularly effective:
- Cognitive Processing Therapy (CPT): This cognitive therapy focuses on identifying and challenging distorted beliefs about the trauma and traumatic memories, replacing them with healthier perspectives.
- Prolonged Exposure (PE) Therapy: Exposure therapy encourages gradual confrontation of trauma-related thoughts, memories, and situations to reduce avoidance and fear over time.
2. Eye Movement Desensitisation and Reprocessing (EMDR)
EMDR is a structured therapy that involves recalling traumatic events while engaging in bilateral stimulation, such as guided eye movements. This technique helps the brain reprocess distressing memories, reducing their emotional intensity. Studies have shown EMDR to be particularly effective in alleviating PTSD symptoms in veterans.
3. Medication-Assisted Treatment
For some veterans, medication can be a valuable component of PTSD treatment, especially when used in conjunction with therapy. Commonly prescribed medications include:
- Selective Serotonin Reuptake Inhibitors (SSRIs): These help regulate mood and reduce anxiety.
- Sleep medication: A medication that can be effective in reducing nightmares and sleep disturbances.
- Mood Stabilizers or Antipsychotics: Used in severe cases where additional symptom management is required.
4. Transcranial Magnetic Stimulation (TMS)
TMS is a non-invasive, safe, evidence-based treatment that uses electromagnetic pulses to stimulate specific brain regions associated with PTSD. This PTSD therapy is gaining traction as an effective alternative for veterans who do not respond well to conventional treatments.
5. Group Therapy and Peer Support Programs
Many veterans benefit from group therapy and peer support programs where they can share experiences, learn coping strategies, and build a sense of camaraderie. Programs like those offered by the Department of Veterans' Affairs, non-profit organisations, and community groups provide essential support networks that aid in recovery.
6. Alternative and Complementary Therapies
In addition to traditional treatments, some veterans find relief from PTSD and other mental health symptoms through holistic approaches such as:
- Mindfulness, Yoga and Meditation: Helps with physical health, emotional regulation and stress management.
- Yoga and Tai Chi: Promotes relaxation and body awareness as well as physical health, reducing symptoms of hyperarousal.
- Equine and Canine Therapy: Interacting with therapy animals has shown to provide emotional comfort and encourage social engagement.
- Acupuncture and Massage Therapy: Can help alleviate PTSD-related physical tension and stress.
The Role of Family and Community Support
Recovery from PTSD is not solely an individual effort—family, friends, and community support play a crucial role in the healing process after a traumatic event. Loved ones can:
- Encourage veterans to seek help from a mental health professional or group therapy without judgment.
- Participate in therapy sessions when appropriate.
- Learn about PTSD to better understand the challenges faced by their veteran family members.
- Provide a stable, supportive, and patient environment.
Veterans’ organisations and community-based support groups also offer vital resources for treating PTSD, including vocational rehabilitation, financial assistance, and social reintegration programs to help veterans rebuild their lives.

Barriers to Treatment and How to Overcome Them
Despite the availability of effective treatments, many veterans struggle to seek help due to stigma, fear of being perceived as weak, or lack of access to mental health services. Addressing these barriers requires:
- Increasing Awareness: Educating veterans and the public about PTSD and the importance of treatment for traumatic memories and other mental health conditions.
- Expanding Access to Care: Ensuring that mental health services are easily accessible, especially in rural or underserved areas.
- Encouraging Open Conversations: Promoting a culture where seeking help from a mental health professional after a traumatic event or traumatic experiences is seen as a sign of strength rather than weakness.
- Leveraging Telehealth Services: Online therapy and virtual counselling can bridge the gap for veterans who cannot easily access in-person care for mental health problems.
Hope and Healing for Veterans with PTSD
Living with PTSD can be challenging, but recovery is possible with the right treatment and support from family, friends, and mental health professionals. Veterans who seek help often find that with time, therapy, and a strong support system, they can reclaim their lives and build a brighter future. It is essential for society to honour the sacrifices of those who served by ensuring they have access to the highest quality mental health care and the compassionate support they deserve.
If you or someone you know is struggling with PTSD or symptoms from traumatic memories, reach out to a mental health professional at Monarch Mental Health Group or a veterans’ support organisation. Help is available from our clinics across Australia, and no one has to face PTSD alone.
FAQs
What treatment options does Monarch Mental Health Group offer for veterans with PTSD?
Monarch Mental Health Group provides a range of evidence-based treatments for veterans, including Cognitive Behavioural Therapy (CBT) and Cognitive Processing Therapy (CPT), Eye Movement Desensitisation and Reprocessing (EMDR), medication-assisted therapy, and Transcranial Magnetic Stimulation (TMS). Our experienced mental health professionals can assess veterans for a PTSD diagnosis and tailor treatments to suit individual needs and manage or reduce mental health symptoms related to a traumatic event.
Is Transcranial Magnetic Stimulation (TMS) available for veterans with PTSD symptoms?
Yes, Monarch Mental Health Group offers TMS therapy, a non-invasive and innovative treatment for PTSD, at several of our clinic locations. TMS is particularly effective for veterans who have not responded well to conventional treatments, and this therapy can be combined with various types of talk therapy, cognitive therapy, psychiatric therapy, and medications if needed.
Does Monarch Mental Health Group accept referrals from the Department of Veterans' Affairs?
Yes, we work closely with the Department of Veterans' Affairs and accept referrals to ensure that veterans receive the best possible care and support. Many of our treatments, including TMS for PTSD and psychological services, are eligible for insurance, Medicare rebates, or DVA benefits. Coverage and eligibility may vary depending on your specific policy or DVA entitlements.
What other support services does Monarch Mental Health Group provide for veterans?
In addition to clinical treatments such as TMS therapy for Post Traumatic Stress Disorder, Monarch Mental Health Group offers peer support groups, counselling for families, and educational resources to help veterans and their loved ones navigate PTSD recovery. We are committed to providing a holistic approach to mental health care and have mental health clinics across Australia.
How can veterans get started with PTSD treatment at Monarch Mental Health Group?
Veterans can book an initial consultation by contacting their nearest Monarch clinic or obtaining a referral from their GP. Our team is dedicated to guiding veterans through the treatment process and ensuring they receive compassionate, high-quality care.
.png)
About The Author
Dr Ted Cassidy
Dr. Ted Cassidy is a psychiatrist and co-founder of Monarch Mental Health Group in Australia, which provides innovative treatments for depression, PTSD, and anxiety. Monarch Mental Health is recognized as Australia's first outpatient clinic offering assisted therapy and is the largest provider of outpatient magnetic stimulation therapy.